What are sexually transmitted diseases (STDs)?
Sexually transmitted diseases (STDs), or sexually transmitted infections (STIs), are infections that are passed from one person to another through sexual contact. The contact is usually vaginal, oral, or anal sex. But sometimes they can spread through other intimate physical contact. This is because some STDs, like herpes and HPV, are spread by skin-to-skin contact.
There are more than 20 types of STDs, including:
- Chlamydia
- Genital herpes
- Gonorrhoea
- HIV/AIDS
- HPV
- Pubic lice
- Syphilis
- Trichomoniasis
What causes sexually transmitted diseases (STDs)?
There are 3 major causes.
- Bacteria, including chlamydia, gonorrhoea, and syphilis
- Viruses, including HIV/AIDS, herpes simplex virus, human papillomavirus, hepatitis B virus, cytomegalovirus (CMV), and Zika
- Parasites, such as trichomonas vaginalis, or insects such as crab lice or scabies mites.
Any STI can be spread through sexual activity including sexual intercourse, and some STIs also are spread through oral sex and other sexual activity. Ejaculation does not have to occur for an STI to pass from person to person.
In addition, sharing contaminated needles, such as those used to inject drugs, or using contaminated body piercing or tattooing equipment also can transmit some infections, such as HIV, hepatitis B, and hepatitis C. A few infections can be sexually transmitted but are also spread through nonsexual, close contact. Some of these infections, like CMV, are not considered STIs even though they can be transmitted through sexual contact.
Regardless of how a person is exposed, once a person is infected by an STI, he or she can spread the infection to other people through oral, vaginal, or anal sex, even if he or she has no symptoms.
Who is affected by sexually transmitted diseases (STDs)?
Most STDs affect both men and women, but in many cases the health problems they cause can be more severe for women. If a pregnant woman has an STD, it can cause serious health problems for the baby.
What are the symptoms of sexually transmitted diseases (STDs)?
STDs don’t always cause symptoms or may only cause mild symptoms. So it is possible to have an infection and not know it. But you can still pass it on to others.
If there are symptoms, they could include:
- Unusual discharge from the penis or vagina
- Sores or warts on the genital area
- Painful or frequent urination
- Itching and redness in the genital area
- Blisters or sores in or around the mouth
- Abnormal vaginal odour
- Anal itching, soreness, or bleeding
- Abdominal Pain
- Fever
How are sexually transmitted diseases (STDs) diagnosed?
If you have a doubt you might have caught one of the above diseases, you should talk to your health care provider about your risk for STDs and whether you need to be tested. This is especially important since many STDs do not usually cause symptoms.
Some STDs may be diagnosed during a physical exam or through microscopic examination of a sore or fluid swabbed from the vagina, penis, or anus. Blood tests can diagnose other types of STDs.
But, if it is difficult to consult a doctor, you can simply purchase a self testing std kit and do the testing on your own. You can easily find the self test kits through the link below.
https://miosalute.com/product-category/std/
What are the treatments for sexually transmitted diseases (STDs)?
Antibiotics can treat STDs caused by bacteria or parasites. There is no cure for STDs caused by viruses, but medicines can often help with the symptoms and lower your risk of spreading the infection.
Correct usage of latex condoms greatly reduces, but does not completely eliminate, the risk of catching or spreading STDs. The most reliable way to avoid infection is to not have anal, vaginal, or oral sex.
There are vaccines to prevent HPV and hepatitis B.
Can sexually transmitted diseases (STDs) be prevented?
Correct usage of latex condoms greatly reduces, but does not completely eliminate, the risk of catching or spreading STDs. If your or your partner is allergic to latex, you can use polyurethane condoms. The most reliable way to avoid infection is to not have anal, vaginal, or oral sex.
There are vaccines to prevent HPV and hepatitis B.
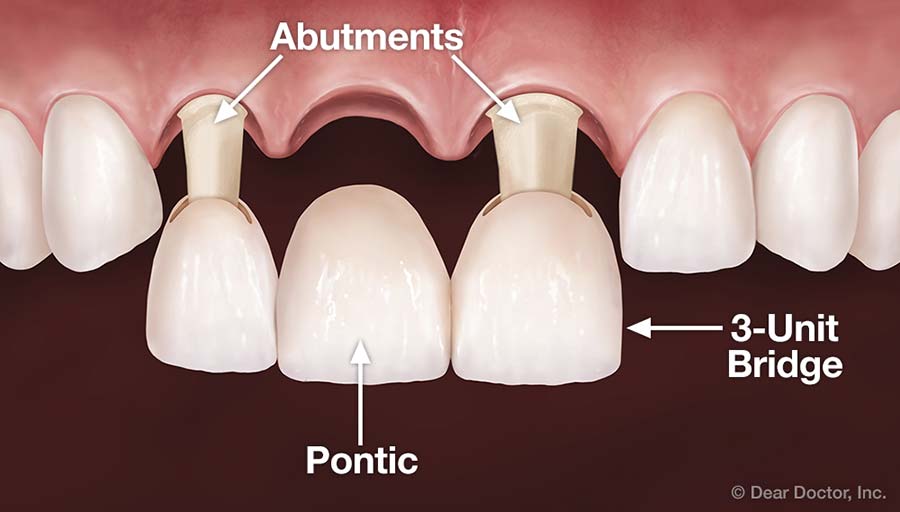
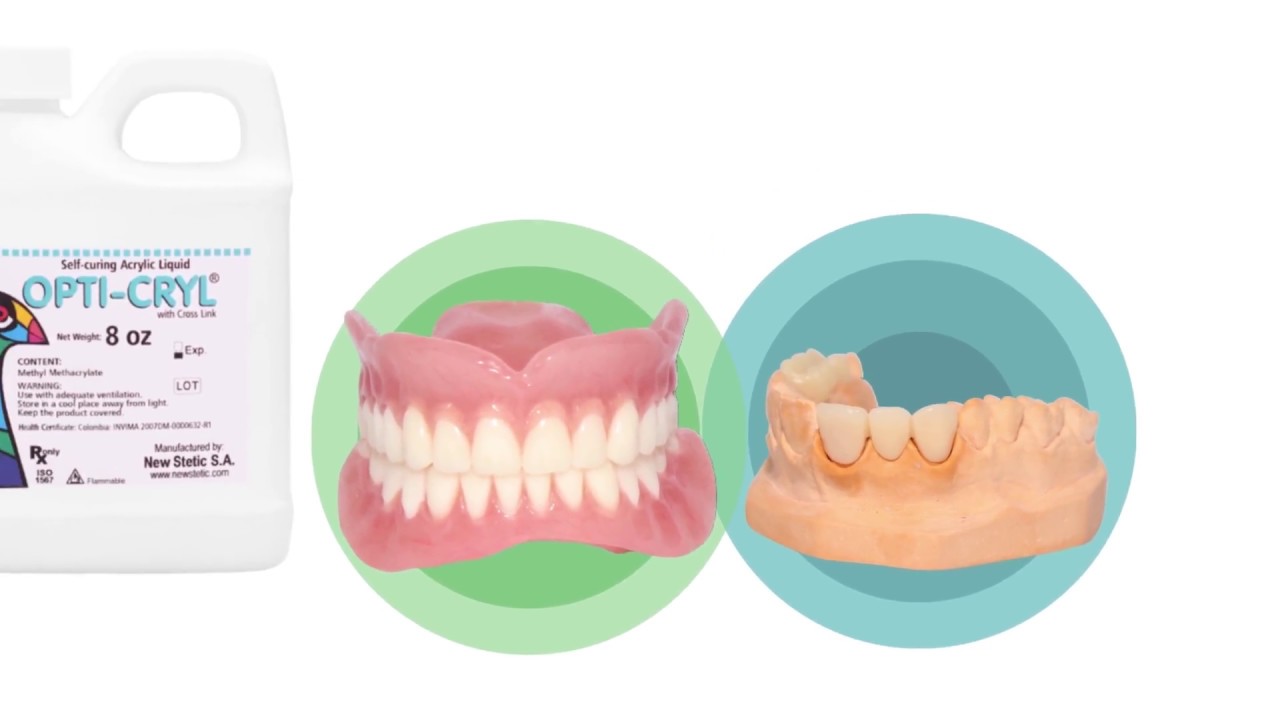
I hope these information provided a ground idea about the diseases. We will try to discuss into details with the upcoming posts. On the other hand, I would like to invite you to read my other articles about Dentistry. And if you are interested you are welcome to go through some of my free lessons. Enjoy!!!